Care for Lung Muscles
The information on this page represents the recommended standard of care for Duchenne muscular dystrophy. Most of the care recommendations also apply to Becker muscular dystrophy, but at older ages. Most, but not all, people with Duchenne are males—but the care recommendations apply to both males and females with Duchenne.
If you don’t understand any of the medical terms and concepts, ask your healthcare providers. Take notes and ask questions during your clinical visits.
Lung facts to remember
- In Duchenne, the muscles responsible for breathing and coughing weaken over time, and may require the use of assistive equipment.
- Antibiotics, extra breathing tests, and assistance with coughing care are needed when there is a respiratory infection.
- People with Duchenne should avoid inhaled anesthesia if at all possible, and should NEVER have the drug succinylcholine, or any derivative of succinylcholine.
- If you are sick or injured and your oxygen saturation drops, your doctor should use caution when giving supplemental oxygen (i.e. through a nasal cannula or mask).
- Lung function should be checked before surgery or undergoing anesthesia.
Pulmonary Awareness Video Series
With the help of an expert team of pulmonologists, parents and people living with Duchenne, and support from Santhera Pharmaceuticals, PPMD has worked to develop a series of Pulmonary Awareness videos.
VIDEO 1: WHAT TO EXPECT AT YOUR PULMONARY VISIT
View all Pulmonary Awareness VideosCoughing and Breathing Muscles
The lungs of people with Duchenne are not directly affected by the disease. However, the muscles responsible for helping you breathe, including the diaphragm, can be greatly affected. The diaphragm sits below the lungs and is the muscle responsible for this crucial movement of air. These muscles gradually weaken over time and cause shallow breathing (hypoventilation) and weaken your cough. This can put people with Duchenne at risk for developing illnesses and infections of the lungs more easily.
Monitoring for Breathing Problems
A pulmonologist (breathing doctor) is a vital member of your neuromuscular care team and it is important to see yours at least once a year. Your pulmonologist will monitor your breathing and coughing strength closely to detect any problems that may arise. They will also order testing to closely examine your breathing and/or coughing strength, as well how you breathe when you are asleep. However, it is important to notify them of any symptoms you are having at home that may indicate you are having difficulty breathing (see below).
Pulmonary Function Testing
All people with Duchenne should have regular pulmonary function testing starting at the time of diagnosis or by ages 5-6. This test uses a mouthpiece connected to equipment that measures your breathing. To learn more about this test and what your pulmonologist is looking for, please visit this page about pulmonary function testing.
Sleep Studies
In general, you breathe more shallow at night than you do while awake. In Duchenne, this can be harmful because you may already have weakened breathing muscles to begin with. If your pulmonologist suspects you may be breathing too shallowly at night (nocturnal hypoventilation) or you may have sleep apnea, they may order a sleep study. To learn more about this test and what your pulmonologist is looking for, please visit this page about sleep studies.
Symptoms of Breathing Trouble
Although your pulmonologist will be monitoring your breathing function through testing, it is important to monitor for signs of difficulty breathing at home. If you are experiencing shortness of breath at any time or it is taking longer than usual to catch your breath, let your pulmonologist know immediately.
In addition, symptoms of problems breathing can often be “silent,” or you may attribute them to something unrelated. If you have one or more of the following symptoms, it may be because you are having trouble breathing. Always notify your pulmonologist if you experience any of the following:
- Snoring
- Feeling tired throughout the day regardless of getting a full night of sleep
- Have headaches in the morning or throughout the day without cause
- Have difficulty paying attention (usually noticed in school)
- Difficulty getting restful sleep, including waking up frequently through the night, having trouble waking up in the morning, or even nightmares
- As you wake up, you can feel your heart pounding
Scoliosis and Breathing
Scoliosis (curvature of the spine) is relatively common in Duchenne. In addition to weakened breathing muscles, scoliosis can also further affect respiratory function. This is because the curve of the spine can impact the structure of the chest wall. If you have scoliosis, you should be referred to an orthopedic specialist to discuss interventions for prevention and treatment.
Other Causes
Constipation is often overlooked in Duchenne and can affect breathing. If your abdomen is too distended, it can make it more difficult to take deep breaths.
Posture and positioning can also be a factor for impaired breathing. Your physical therapist and occupational therapist can work with you to ensure a correct posture is supported in your wheelchair or other seating.
Recommended Care For All Ages
Prevention
Vaccinations
In general, it is important to be up-to-date on the recommended vaccination schedule. People with Duchenne are at a higher risk for pneumonia due to weakened cough, which clears the lungs of illness-causing bacteria and viruses. It is important for the pneumonia vaccine to be given by age two and repeated as advised by your primary care provider.
It is important for you and your entire family to have the flu shot every year. The flu can be especially harmful for people with Duchenne. It is important to vaccinate those close to you to lessen the risk of exposure.
Oral Care
Oral hygiene is very important to prevent bacteria in the mouth that can cause chest infections. Consider using products such as toothpaste or other oral cleaning products that contain chlorhexidine. Additionally, be sure to visit your dentist on a regular schedule.
Coughing and Managing Mucus
Your lungs produce mucus to trap the dust and particles we normally breathe in every day. It is important to remove this mucus with these germs from your lungs to prevent respiratory illnesses from happening. This is done by coughing. In Duchenne, your cough can become weak, and it may be more difficult to remove this mucus from your lungs. The inability to remove mucus (secretions) from your lungs puts you at risk for pneumonias or other respiratory infections.
There are several ways to assist your cough, both manually and with a machine. However, managing your secretions efficiently may help you to clear these secretions from your lungs as well.
If your secretions are thick and too dry, it is a good idea to use humidification. This can help thin out the mucus, making it easier to cough up. Antihistamine medications such as those used for allergies are also ok to use. However, it is NOT recommended to use decongestants. A good rule of thumb is if there is a “-D” in the title, avoid taking this medication.
Acute Respiratory Illnesses
People living with Duchenne who have a weaker cough, are at a higher risk for respiratory illnesses and potentially pneumonia. If you or your child has a cough assist machine or manual bag, it is important to use these consistently, especially during times of respiratory illnesses. When assisted coughing is begun, a pulse oximeter should be kept at home. If pulse oxygen saturation drops lower than 95% in room air, it is important to increase how often you are assisting cough.
During acute respiratory illnesses, antibiotic therapy should be added for patients who have 3 of the following 5 clinical signs of pneumonia:
- Fever
- Elevated white blood cell count or C-reactive protein level
- Sputum (thick mucus or “phlegm”) production
- A pulmonary infiltrate (dense area) on chest x-ray
- Hypoxemia (below normal oxygen saturation) or respiratory distress
Emergencies, Surgeries, and Hospitalizations
In the case of a respiratory emergency, it is important to know what to do. You should avoid all inhaled anesthesia, most specially the drug succinylcholine, or any derivative of succinylcholine as it is not safe for use in Duchenne. Most IV anesthesia is safe for use during procedures. Learn more about precautions for surgery & anesthesia in Duchenne.
If your oxygen saturation drops for any reason, your doctor should use caution when administering supplemental oxygen (i.e. through a nasal cannula or mask). You should be monitored closely and oxygen should be given for the shortest time period possible.
Be sure to bring any breathing equipment you use at home (BiPAP machine, cough assist machine) with you to the hospital. Oftentimes these machines are not available on hand at the hospital. It is also important that you continue to use these if admitted to the hospital so your illness does not get worse.
Your lung function should also be tested before any type of surgery or undergoing anesthesia. Additionally, make your pulmonologist aware anytime you plan to undergo surgery or procedure.
Recommended Care By Stage
To view comprehensive care by stage, please click here.
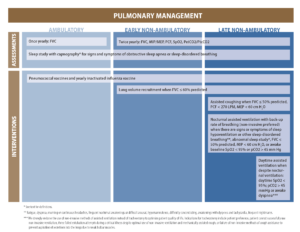
Ambulatory Stages (Diagnosis – Around 9, still walking)
Children in this stage usually do not have any problems breathing . However, it is important to take your child to a pulmonologist to have pulmonary function tests once a year. It is a good idea to start these tests young so your pulmonologist can have baseline records as well as Keeping a copy of your child’s latest breathing tests to show other healthcare providers is a good idea.
If your child gets sick, especially with a cold or chest infection, make sure they receive antibiotics and take them to the doctor for extra breathing tests. Even if they have not needed assistance coughing before, they may require techniques to assist coughing during illness.
Non-Ambulatory Stages (Around Age 10 – Adulthood, unable to walk without assistance)
Breathing muscles will become weaker as you get older. The diaphragm is a muscle under the lungs that helps with breathing and supports taking deep breaths. Some people with Duchenne develop diaphragm weakness at this stage. This can cause difficulty taking deep breaths and expanding the lungs completely. After a person with Duchenne stops walking, they may have trouble coughing and require assistance.
Pulmonary function tests should continue to be done at least once a year to trend monitor the strength of the breathing muscles. When FVC is less than or equal to 60% predicted, lung volume recruitment (manual or with a cough assist machine) is indicated to preserve respiratory function. However, it is important to talk to your pulmonologist about how to monitor for symptoms of difficulty breathing at home. Keep a copy of your latest pulmonary function tests on hand in case of an emergency or to share with your other neuromuscular care team providers.
If you get sick, especially with a cold or chest infection, make sure to take antibiotics as needed, perform breathing tests more frequently to evaluate breathing, and use assistance (manual or with a cough assist machine) with coughing. You may also need to use a breathing machine (ventilator) for a while, even if you have not used one before.
If you are showing any signs or symptoms of decreased oxygen during sleep, your pulmonologist should order a sleep study. If the sleep study shows that there is impaired breathing during sleep, using non-invasive ventilation can help breathing and increase oxygen during sleep.
The BiPAP machine is the most commonly used form of non-invasive ventilation in Duchenne. The BiPAP machine delivers two different pressures through a mask that helps to keep your airways open, allowing you to breathe easily and more comfortably during sleep. If your breathing muscles become increasingly weakened, you may eventually need to use this during the day as well.
The DMD Pathfinders, a user-led charity from the UK who work to promote choice and control and quality of life for teenagers and adults living with Duchenne, has developed a series of advice guides and has kindly given PPMD permission to share with our community. The DMD Pathfinders developed a series of Ventilation Frequently Asked Questions (FAQ) to address common questions and concerns on respiratory and ventilation issues. In addition, when daytime ventilation is required, it is important to prepare for emergency stations such as power failure, which is discussed in Life and Breath – Managing Ventilation and Power Failure.
A weakened diaphragm can also result in a weak cough, which decreases your ability to clear secretions out of your lungs and may result in more lung infections, and even pneumonia. During pulmonary function testing, the respiratory therapist will also measure the “cough peak flow.” If coughing becomes weak, methods to regularly assist cough should be discussed with your pulmonologist.
Assisted Cough vs. “The Vest”
“The Vest,” or “high frequency chest wall oscillation,” is a technology employing an inflatable vest connected by an air hose to a pulse generator. The vest rapidly inflates and deflates, applying gentle pulsed pressure to the chest wall. The aim is to generate “shearing force” between the mucus and the lining of the airways, with the intention of dislodging these secretions that can subsequently be coughed and cleared.
Vest therapy is ideal for patients who have conditions with abnormally thick mucus (such as cystic fibrosis, COPD, chronic bronchitis, etc). Patients with respiratory muscle weakness, however, do not typically have abnormally thick mucus. Their difficulty lies in the inability to clear mucus of normal consistency. Therefore, vest therapy is rarely appropriate for patients with Duchenne. Its use may be instituted during the recovery of an extensive pneumonia or if there is a stubborn area of collapse. That would be at the discretion of the treating physician.
The “cough assist” uses a facemask, mouthpiece, or tracheostomy to deliver gradual positive air pressure to the airway (inflation), followed by a rapid shift to negative air pressure (deflation), in an attempt to simulate a natural cough. As patients with Duchenne have difficulty clearing secretions, a cough assist is not only appropriate therapy, but is critical for maintaining pulmonary health and reducing the incidence of infections and pneumonias.
Some criticisms of the cough assist machine are that it is big, bulky, heavy, and difficult to travel with. New machines are on the market, which are smaller, lighter, and more convenient. Be sure and ask if these newer options are available through your provider. Also, these machines need to be calibrated appropriately for the patient using them. Please be sure to ask for instruction when the machine is delivered to your home.
Effective assisted cough techniques should be taught early, certainly when peak cough flow (PCF) falls below 300 lpm and/or used during a respiratory illness. For more information regarding cough assist, click here.