
Every single person living with Duchenne deserves the best care possible. It is important that families know who is in charge of delivering the care they need and understand what centers are providing optimal, standardized care and services in agreement with the Duchenne Care Guidelines.
PPMD’s Certified Duchenne Care Center (CDCC) Program helps to ensure that centers comply with the standards of care and services that have been established in the Duchenne Care Guidelines. All CDCCs have met the requirements for, and agree to provide, optimal standardized care and services.
While 2021 brought with it another year of pandemic life, PPMD and our CDCC Program forged ahead with a year full of progress, including virtual opportunities and events for the CDCC community.
2021 Program Highlights
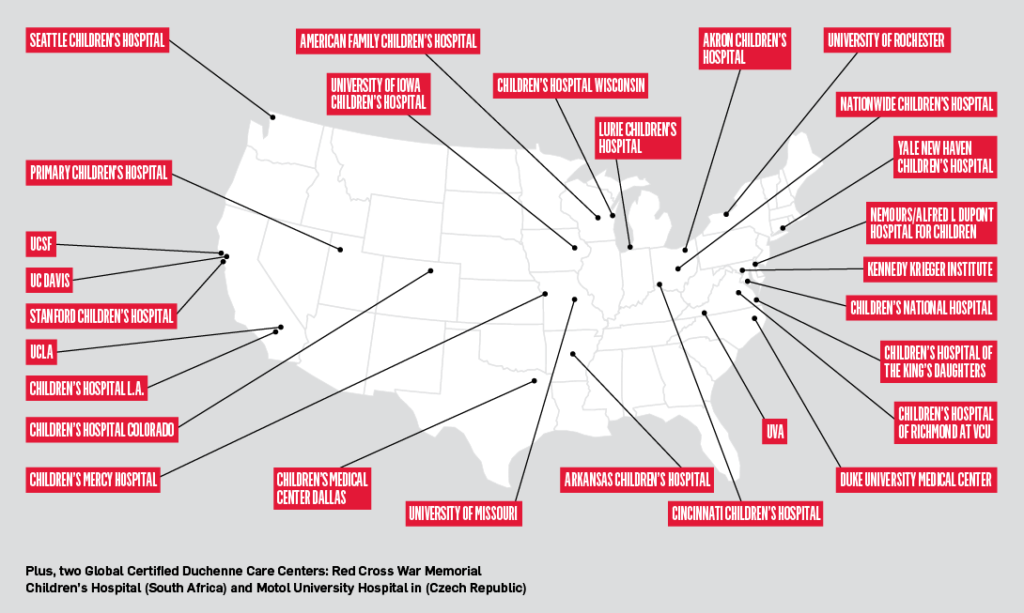
PPMD is thrilled that the CDCC Program served more than 3,700 patients with Duchenne and Becker in 2021. This number grows year after year, with patients seeking their regular Duchenne care at one of our 28 Certified Centers reaching from coast to coast.
While pandemic restrictions inhibited us from granting additional certifications in 2021, we were pleased to resume site visits in Fall 2021 and look forward to completing many more in 2022.
The program currently has 11 site visits scheduled, 10 additional sites in our CDCC pipeline, with three certifications pending.
Living in a Virtual World
While we were unable to gather in January for our annual Duchenne Healthcare Professionals (HCPs) Summit, PPMD created and launched a brand-new resource targeted to HCPs, the Duchenne Professionals Masterclass. This new resource was launched via a series of live, interactive sessions in late winter 2021, and the PPMD team is eager to continue to utilize and evolve this platform for professional development for HCPs and other experts caring for people living with Duchenne.
If you are an HCP caring for patients with Duchenne and are interested in learning more about the Masterclass and access to discounted pricing, please email masterclass@parentprojectmd.org.
Inaugural Inter-Institutional Collaboration Grant
Additionally, PPMD was happy to fund two inter-institutional collaboration grant awards. The awards require that proposed projects include collaboration between a minimum of two certified centers with awards of up to $150,000 per project over a two-year period (Spring 2021- Spring 2023).
- The first, awarded to Dr. Chet Villa and the ACTION network, whose 50 member centers include 18 CDCCs, are investigating shared decision making and outcomes in Duchenne cardiac care.
- A second award to Dr. Rachel Thienprayoon and the Ohio Pediatric Palliative and End-of-Life Care Network (OPPEN), which includes Cincinnati Children’s Hospital, Nationwide Children’s Hospital, and Akron Children’s Hospital (all CDCCs), is developing a patient- and family-centered educational tool to help visualize trajectory, improve patient agency and adherence with medical recommendations, and improve quality of life and future planning for patients and caregivers.
A community update on these projects will be available this summer as part of the 2022 PPMD Annual Conference.
 A Growing Team
A Growing Team
Spring brought with it the addition of Dr. Mena Scavina to the PPMD team as part-time CDCC Program Advisor. Dr. Scavina is also the director of the Duchenne clinic and Certified Duchenne Care Center at Nemours Children’s Health in Wilmington, Delaware.
Dr. Scavina was a welcome addition to the team, and will work on several programs supporting the care of all people affected by Duchenne, with emphasis on women carriers of Duchenne and Becker.
Looking Ahead
Finally, in the fall and after another wave of covid eased its grip, we were happy to resume CDCC site visits for the first time since 2019. We are eager to continue the expansion of the Certified Duchenne Care Center program, and excited to see what 2022 has in store for the Duchenne community!
The Community Voice is Critical
Your voice is a critical component to the continued excellence of care provided at centers within the CDCC network. One way to get involved is the annual completion of the Clinical Experiences Survey. This survey lets the CDCC Certification Committee know what elements of care and services you receive, what is going well, and where PPMD can help advocate for improvement in the delivery of care and services at your center.
Responses are collated per center, and at the end of the year, each center receives an anonymized report of their own center, as well as one representative of the network as a whole. This supports centers in the process of continuous improvement to ensure you receive the best care possible.
Your voice is an integral part of this process! Complete the survey here.
PPMD is Here For You!
In addition to the services provided from the expert clinicians at all of the CDCCs, PPMD is here to come alongside you and offer support however we can. Whether navigating a new diagnosis, finding a referral, basic medical guidance, assistance navigating resources, benefits, education, genetic counseling, or more, we are here for you! Schedule a time to meet with the PPMD Care Team or one of PPMD’s genetic counselors via their office hours, and let us help!
Reminders for Parents in an Emergency
- Take the PPMD emergency card with you
- Take a copy of the summary of your last neuromuscular visit with you or a brief 1 page summary of your/your child’s care
- Download, and keep handy, the PPMD mobile app
- Reference the PJ Nicholoff Steroid Protocol for stress dosing recommendations, and share with your medical team
- Take any equipment that you use at home (cough assist, BiPAP, etc.) and medications that you take, with you
- Take a copy of your last ECG with you. (All people living with Duchenne have an abnormal baseline ECG. Providing the emergency team with your baseline heart rate and rhythm will help them to know if anything has changed.)
- Keep the information regarding oxygen use and appropriate anesthesia available for you and the emergency room staff
- Call your neuromuscular team and let them know what is happening
- Be sure that your neuromuscular team is talking with the emergency staff and are guiding your care
- If you/your child has developed an “emergency care plan,” take that as well
2021 ANNUAL REPORT FOR CDCC MEMBER CENTERS
The table below describes the 2021 annual report for each center.



 by: Parent Project Muscular Dystrophy
by: Parent Project Muscular Dystrophy

