On Monday September 9, PPMD along with I-ACT for Children and the Duchenne Regulatory Science Consortium (DRSC) held an open meeting inviting all stakeholders (patients, families, industry sponsors, and regulators) in Duchenne to learn and comment on a new type of clinical trial, the Duchenne Platform Trial.
Currently the protocol for the Duchenne Platform Trial is being co-drafted by members of the three convening organizations with input from scientific experts. This meeting captured the input of all the other stakeholders in the Duchenne community.
What is the Duchenne Platform Trial?
The Duchenne Platform Trial is an alternative to current clinical trial design, developed to help accelerate clinical trial testing. Typically, for each trial a sponsor needs to go through a laborious process of identifying and vetting sites for their trial, acquiring IRB approval, training the staff on the protocol, and then recruitment of a small sub population of the Duchenne community.
The Duchenne Platform Trial utilizes a master protocol that will greatly reduce these initial development times, so investigational products can be evaluated sooner. Additionally, because of the standardization and shared randomization across sites, patients assigned to placebo can be pooled, which means that less patients need to be enrolled overall, and of those less are assigned to placebo. Each investigational product joins the trial as a new arm, rather than having to recreate new trial infrastructure for every product. Sponsors won’t have to build a house from the ground up for every investigational product – they can just rent a room.
Why a platform trial?
Despite the years of investment into drug development in the Duchenne space, our community only has two approved therapies. This is simply not good enough. Disruptive innovation is needed to deliver better treatments for Duchenne more quickly. We have a strong development pipeline; we must find out, faster, if these drugs work. PPMD feels the development of the Duchenne Platform Trial will be beneficial for all stakeholders in the community. Here are some of the benefits of the Duchenne Platform Trial:
| Broader inclusion criteria | This expands the restricted population normally recruited for trials to a broader portion of the population. |
| One-time enrollment | Once a patient is enrolled they are randomized to a drug arm. Should that drug fail, the patient isn’t removed from the trial, they are re-randomized to a different arm. |
| Extending the timeframe for participating in trials | Once enrolled in the trial, if the drug a patient is on fails they are re-randomized to a different drug in the trial. This also means that a patient isn’t aging out of clinical trials or restricted because of a loss of ambulation. |
| Less placebo | The randomization to placebo is 3:1 because all of the sponsors in the trial share placebo data, meaning higher chances of receiving drug. |
| Faster failure | With standardized outcome measures and a shared placebo arm, drugs that aren’t efficacious can be recognized and removed from the trial faster and those patients can be re-randomized to another drug that may provide benefit. We don’t want people with Duchenne to stay in a clinical trial where the drug they are receiving is providing little-to-no benefit. |
| Combination therapy | A platform trial is the best environment to begin testing combinations of drugs to see if the incremental increases in treatment can synergize to provide more benefit. |
| Improved standard of care | As drugs are approved, the platform trial is well suited to incorporate those new therapeutics as standard of care so that patients don’t have to wait or worry about delaying their access to beneficial treatment. |
An Alternative Trial Design
It is important to recognize that the Duchenne Platform Trial will not replace all clinical trials or impact current trials that are ongoing or enrolling patients today. Some sponsors may wish to test some investigational products in the Duchenne Platform Trial, while others may not. In its first iteration, compounds or biologics that are intended to express dystrophin (exon skipping, nonsense read-through, or micro-dystrophin) are unlikely to be included in the Duchenne Platform Trial. Rather the Duchenne Platform Trial will first focus on what happens in the absence of dystrophin or referred to as ‘downstream’ approaches. These would include therapies that prevent fibrosis, restore energy to the cell, improve muscle growth, reduce inflammation, and/or protect the heart. Additionally, no one in the community will be forced into the Duchenne Platform Trial. If a family decides they would rather participate in a separate clinical trial they can. This is an alternative trial design that PPMD, I-ACT, and DRSC feel will enhance standard of care and treatment for participants and result in shortened clinical trial times.
FDA Perspective
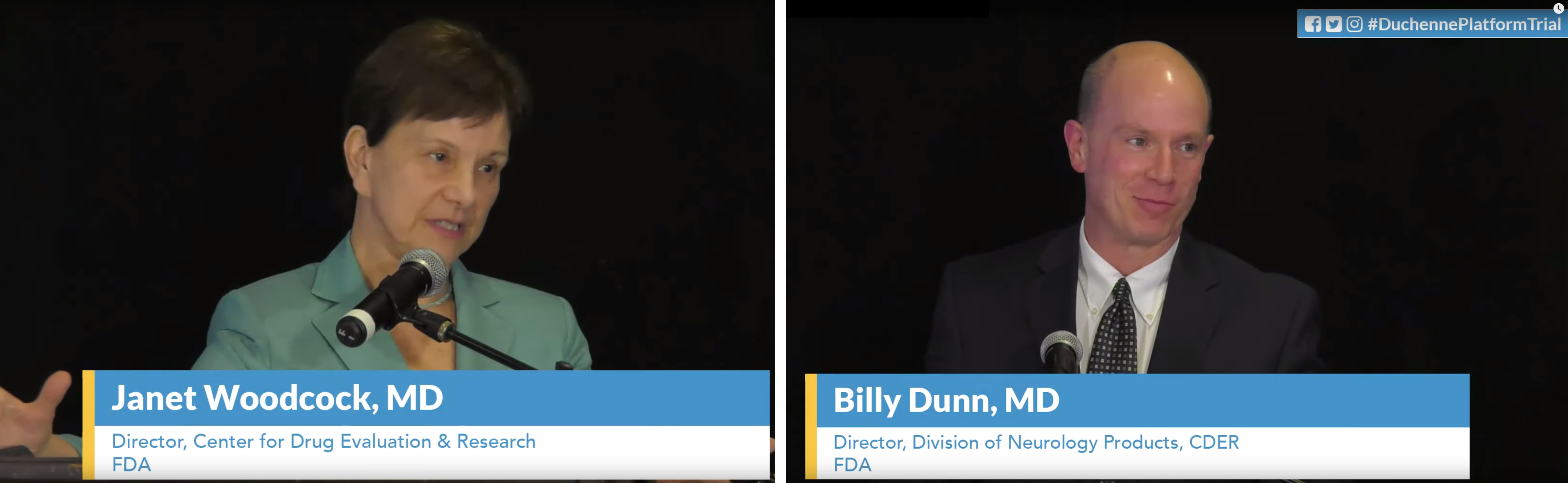
Two Directors from the FDA’s Center for Drug Evaluation and Research were in attendance to share their views on the opportunities presented by a platform trial. Drs. Janet Woodcock and Billy Dunn commented on the potential improvements of the Duchenne Platform Trial compared to traditional placebo controlled trials. The broader inclusion criteria can lead to faster enrollment and broader labelling for approved therapies. The members of the FDA reiterated that the Duchenne Platform Trial’s shared placebo group can reduce burden for families concerned about not receiving drug, help expedite enrollment, and increase a studies power to fail faster. Overall, they believe that the Duchenne Platform Trial will result in increased trial efficiency as it continues to evolve and progress over time.
Inclusion/Exclusion Considerations
Below are the initial inclusion/exclusion considerations for the master protocol of the Duchenne Platform Trial. PPMD, I-ACT, and DRSC are still collecting feedback from sponsors, regulators, clinicians, and of course the patients and families. Some of what is shared below may change before launch. And even after the Duchenne Platform Trial begins, it is expected that elements of the protocol will be revisited over time. The goal is to be as encompassing as possible while maintaining the ability to show efficacy of investigational products.
| Inclusion Criteria |
|
| Exclusion |
*Each new arm may have specific exclusion criteria typically relating to drug efficacy. For instance a respiratory drug may have no benefit in a young child where pulmonary function hasn’t been impacted by disease progression. |
Outcome Measures
Similar to the inclusion/exclusion criteria, the outcome measures initially selected are meant to encompass all aspects of Duchenne. By covering the different areas of the disease, a sponsor can specify which outcome is their primary and have the corresponding data from all the shared placebo arms. Below are the proposed core efficacy assessments/endpoints:
| Lower Limb Functional testing (Ambulatory patients only) |
|
| Upper Limb Functional testing |
|
| Pulmonary function testing/spirometry |
|
| Cardiac Testing |
|
| Quality of Life |
|
Two panels were held to discuss these different outcome measures that were initially selected. As the Duchenne Platform Trial continues to be revised before launching, it is likely that feedback from all stakeholders will influence what is evaluated. Over the course of the two panels, a number of suggestions were made that could further streamline the selected measures. The main focus is to be able to have functional data from every patient regardless of stage of disease.
Other Disease Insights
During the panel on governance, we were able to hear insights from a Marianne Chase, Director of Research Operations, Neurological Clinical Research Institute at Massachusetts General Hospital. She is leading the creation of a platform trial in amyotrophic lateral sclerosis (ALS). The ALS community felt that since no one can predict which drugs will be effective, it is better to reduce placebo and get patients on an investigational product to speed up the timeline for drugs in the ALS pipeline. Marianne’s team is working with the FDA and is aiming to launch their platform trial in the first quarter of 2020 with three drugs in the study. ALS is not the only disease where these trials are being deployed. A number of cancer platform trials are active, such as I-SPY2 trial in breast cancer, Lung-MAP for squamous cell lung cancer, and Beat AML for acute myeloid leukemia, all of which are working towards finding cures for their community faster.
Education and Transparency
Finally, a point that was reiterated more than once during the town hall section of the meeting, was the need for education and transparency on the Duchenne Platform Trial. We want to ensure the entire community is well informed of what the Duchenne Platform Trial is and isn’t. The stakeholder meeting is available online to be viewed. Other educational materials are being developed and a plan for continued community engagement is being considered, including roles on Steering Committees and Community Advisory Boards. The master protocol is currently being revised based on feedback from the stakeholder meeting, with plans to share with the community when the next version is ready. PPMD wants to ensure the voice of all stakeholders in the community are recognized in this process and we will continue to have more opportunities for the community to voice their opinion as development continues to move forward.
Meeting Recording
Welcome & Introduction
FDA Opening Remarks
DPT Protocol in Practice
Overview of DPT Proposed Protocol
Panel 1 – Protocol Objectives & Eligibility
Panel 2 – Endpoints & Schedule of Events
Panel 3 – Operations & Governance
Parent Commentary & Advocacy Perspective



 by: Parent Project Muscular Dystrophy
by: Parent Project Muscular Dystrophy