Contractures & Scoliosis
Orthopedics is the subspecialty that offers surgical and non-surgical devices and procedures to help keep the bones in their proper position and alignment. Orthopedists work closely with physical therapists, physical medicine and rehabilitation specialists (PM&R, “physiatrists”), and orthotists (specialists who make splints and braces). There are several issues that can arise in Duchenne that may benefit from the services of orthopedics.
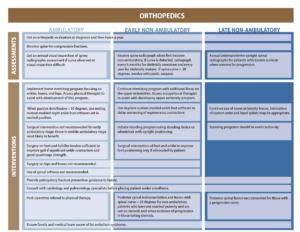
Below is a graph visually showing the orthopedic recommendations from the updated Care Considerations.
PPMD also recorded a webinar addressing Orthopedic Complications in Duchenne that you can listen to:
Contractures
Skeletal muscle attaches to the tendons and joints of the body. In Duchenne, skeletal muscle is replaced by fat and scar tissue. The fat and scar tissue that replace the skeletal muscle are shorter and less flexible. These shorter muscles pull on tendons, that then pull joints into a “flexed” position. If the joint is left in this position too long, the joint becomes “contracted” or permanently fixed in this position. In Duchenne, tightness first develop in the ankles, due to the shortening of the calf muscle and pull on the Achilles tendon.
Learn more about Physical Therapy and Prevention/Non-surgical Management of Contractures here.
Surgical Options for Contracture Management
Tight Achilles tendons can sometimes be surgically “released.” Releases may either be partial or total releases. A partial release involves making small incisions in the Achilles tendon so that it is partially released from the ankle, allowing the tendon to stretch further, giving the ankle further range of motion. A total release involves cutting the Achilles tendon. This completely releases the Achilles tendon from the ankle so that the ankle and foot can be realigned in the proper position.
Following a partial surgical release, it is critical that weight bearing begin immediately. This allows the partially released tendon to begin to stretch. Patients are placed in short leg casts for about two weeks, then are braced for six weeks. This allows the stretch to continue and prevents further contraction of the Achilles tendon. After this process, maintaining that stretch with night braces is extremely important.
Scoliosis
In the normal course of Duchenne—in the absence of steroids or assisted walking—it is likely that scoliosis (or curvature of the spine) will develop within two years of being in a chair full-time. Research suggests that up to 90% of boys not using steroids will develop scoliosis. With the use of steroids, the incidence of scoliosis has been significantly reduced. Your physical therapist and rehabilitation team may be the best to person to monitor the spine, as he or she is likely to see you more often than your medical specialists and will be able to detect early change.
Neuromuscular scoliosis is caused by weakness of the spinal muscles, causing the spine to curve to one side or the other, and generally happens after the loss of ambulation (the ability to walk). While you are ambulatory (still able to walk), the spine should be checked clinically at each neuromuscular visit. When ambulation is lost, a baseline spinal X-ray is encouraged. X-rays are recommended every year, and should be managed in the following way:
Spine X-Rays
- The purpose of the X-ray is to measure the “Cobb angle” – amount of curve in the spine
- Repeat the spinal X-ray each yearly if curve is <15-20 degrees
- Repeat the X-ray every 6 month if curve is >20 degrees
Consider surgery if:
- Progression of scoliosis continues
- There is evidence of vertebral fractures
- Pain
Spinal Fusion Surgery
Spinal fusion surgery connects the individual bones (vertebrae) in your spinal column so they don’t move. During the surgery, rods are placed in the spine that hold the vertebrae together until they “fuse” or grow together. This surgery can help straighten a curve in your spine (scoliosis) or keep it from getting worse. It may relieve pain from broken spinal bones and breathing problems caused by scoliosis. Studies have shown that repairing scoliosis has improved both quality and quantity of life.
While there is generally a high rate of success with this procedure, having scoliosis surgery done at a Certified Duchenne Care Center or a center familiar with the surgical correction of Duchenne scoliosis is important.
Surgeons generally follow the “30-30 Rule”
- If the Cobb angle is >30 degrees and the FVC is >30% of normal, then repair the scoliosis, however the use of NIV and airway clearance has made scoliosis repair possible with FVC’s down to 20%
- Reason to repair scoliosis: longer life
- Scoliosis should be managed irrespective of skeletal maturation
Having spinal fusion surgery may decrease the range of motion of your spine, making it more difficult to lift your arms to your mouth and face. Prior to surgery, it is important to talk with your physical and occupational therapy teams about how this surgery may impact your daily functioning. Consider discussing things like:
- What kind of equipment will you need after the surgery?
- Order the equipment and practice with it before surgery. This will help your adjustment after surgery.
- The decreased range of trunk flexibility after scoliosis surgery usually causes difficulty with self-feeding. Your PT and OT may have suggestions (ie, higher surfaces for your arm, mobile arm support, etc.) to help.
Scoliosis surgery is generally long and complex. It is important to make sure that you and your team are aware of, and are addressing, the surgical issues that are important in Duchenne.
Fractures
Because the bones of people living with Duchenne become very thin and fragile, fractures (broken bones) are extremely common. In fact 20-44% of all people living with Duchenne will break a bone, most likely a bone in the leg. Most fractures generally happen after ambulation is lost and may occur with very little trauma (a bump, changing position, being lifted, etc.).
Fractures frequently occur in the long bones of the body (legs or arms) and in the vertebrae (tiny bones that make up the spine). Fractures in the vertebrae are called “vertebral compression fractures” and should be screened for regularly.
While most fractures can be easily managed, some fractures can have serious results (ie, fat embolism syndrome, loss of ambulation, etc.). Preventing falls will go a long way to helping to maintain ambulation. Inside, making sure areas are as free from clutter, slippery surfaces or fall hazards, as possible, is helpful. Outside, paying attention to uneven surfaces and slippery surfaces can also help to prevent falls. And, again, if you are on a mobility device, wear your seatbelt!





