Care for Respiratory Illness
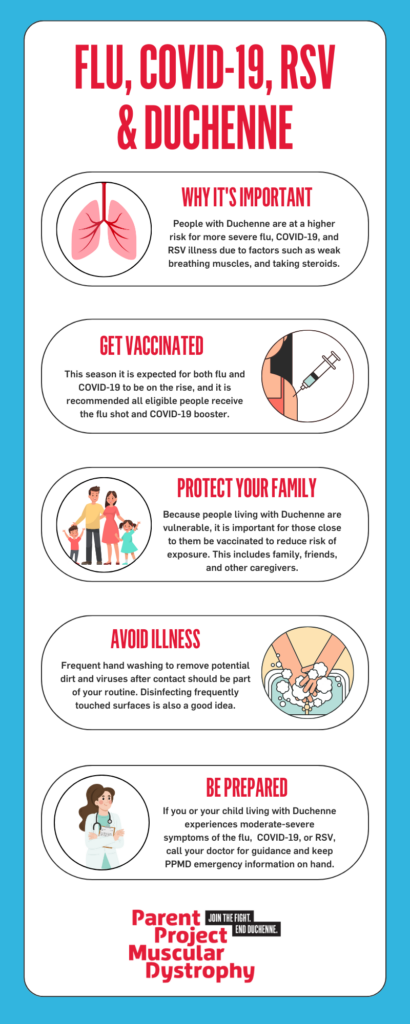
Because respiratory muscles can be weakened in individuals with Dystrophinopathy (Duchenne and Becker), it may be more challenging to fend off infections resulting in increased risk of respiratory complications such as pneumonia. There are several ways you can minimize the risk of developing respiratory illnesses like influenza (flu), COVID-19, RSV and the common cold.
Respiratory Illness Prevention
 Vaccinations
Vaccinations
Vaccinations against influenza and COVID-19 are the best way to prevent infections from these viruses. While it cannot be 100% guaranteed, vaccination has been proven to result in fewer cases of influenza & COVID-19 and milder, shorter illness for those who do become infected with these viruses.
Because people living with Duchenne and Becker are more vulnerable, it is important for those close to them to be vaccinated to reduce risk of exposure. This includes family, friends and other caregivers. Vaccinating family members can reduce your risk of becoming ill, even if you are not vaccinated yourself.
Discuss your eligibility for vaccinations with your neuromuscular doctor and/or primary care provider.
Influenza Vaccines
Each year, everyone six months of age and older needs to be vaccinated against influenza (flu) by the end of October, if possible. Protecting people living with Duchenne & Becker is especially important. A 2005 study done by the CDC found that children with neuromuscular disease are at a six-times greater risk of flu-related respiratory failure. So please vaccinate yourself, your child, and all members of your family.
In the United States, the Centers for Disease Control and Prevention (CDC) developed a vaccine that includes protection against the strains of influenza that were most prevalent in Australia the season before. These vaccines are provided to the public with varying degrees of success. Getting the flu vaccine doesn’t guarantee you won’t get the flu, but it does protect you against the strains the CDC expects to be the biggest threat. Additionally, if you do catch one of those strains, your illness is likely to be milder because you’ve been vaccinated.
There are different types of vaccines for influenza. Vaccinations, including influenza vaccines, are discussed in detail on this page. People living with Duchenne & Becker, especially those who take steroids, should only receive the injectable influenza vaccine, rather than the live virus nasal spray.
COVID-19 Vaccines
Individuals with Duchenne and Becker are at a higher risk of respiratory and cardiac complications from the COVID-19 virus. Because of these risks, it is recommended that individuals and their family members are vaccinated against COVID-19. Additional boosters should be discussed with your primary care provider and/or neuromuscular provider.
For the most up to date information on COVID-19 vaccinations, visit the Centers for Disease Control (CDC)or American Academy of Pediatrics (AAP).
Pneumococcal Vaccines
Pneumococcal vaccines are an inactivated vaccine and are recommended to individuals who are at an increased risk of pneumococcal disease. This is important for individuals with Duchenne and Becker to help reduce risk of bacterial pneumonia years from now. Read more about pneumococcal vaccines here
Other Vaccines
While there are FDA-approved vaccines for RSV, they are currently only approved for adults ages 60 years and older, mothers during pregnancy, and babies up to 8 months old born during or entering their first RSV season.
Read more about CDC recommendations for the flu vaccine and COVID-19 vaccines or ask your healthcare provider for more information. Additional information on vaccinations for individuals with Duchenne and Becker can be found here.
Avoid illness
Good hand hygiene is the most effective way to prevent illness from spreading. Make it a habit for the whole family to wash hands with soap and water, especially before eating, after using the bathroom, and after coming home from school or errands. If soap and water is not available, use an alcohol based hand sanitizer. It is also important to wipe down high-touch surfaces such as wheelchairs, table tops, desks, phones, and tablets. Droplets containing germs can live on these surfaces and can put individuals at risk of infection.
If you are able to avoid others who are sick, it can decrease the risk of viruses spreading to you and/or your family. If you are unable to avoid others who are sick, or are sick yourself, consider wearing a mask to decrease the risk of infection spread.
Respiratory Illness Symptoms
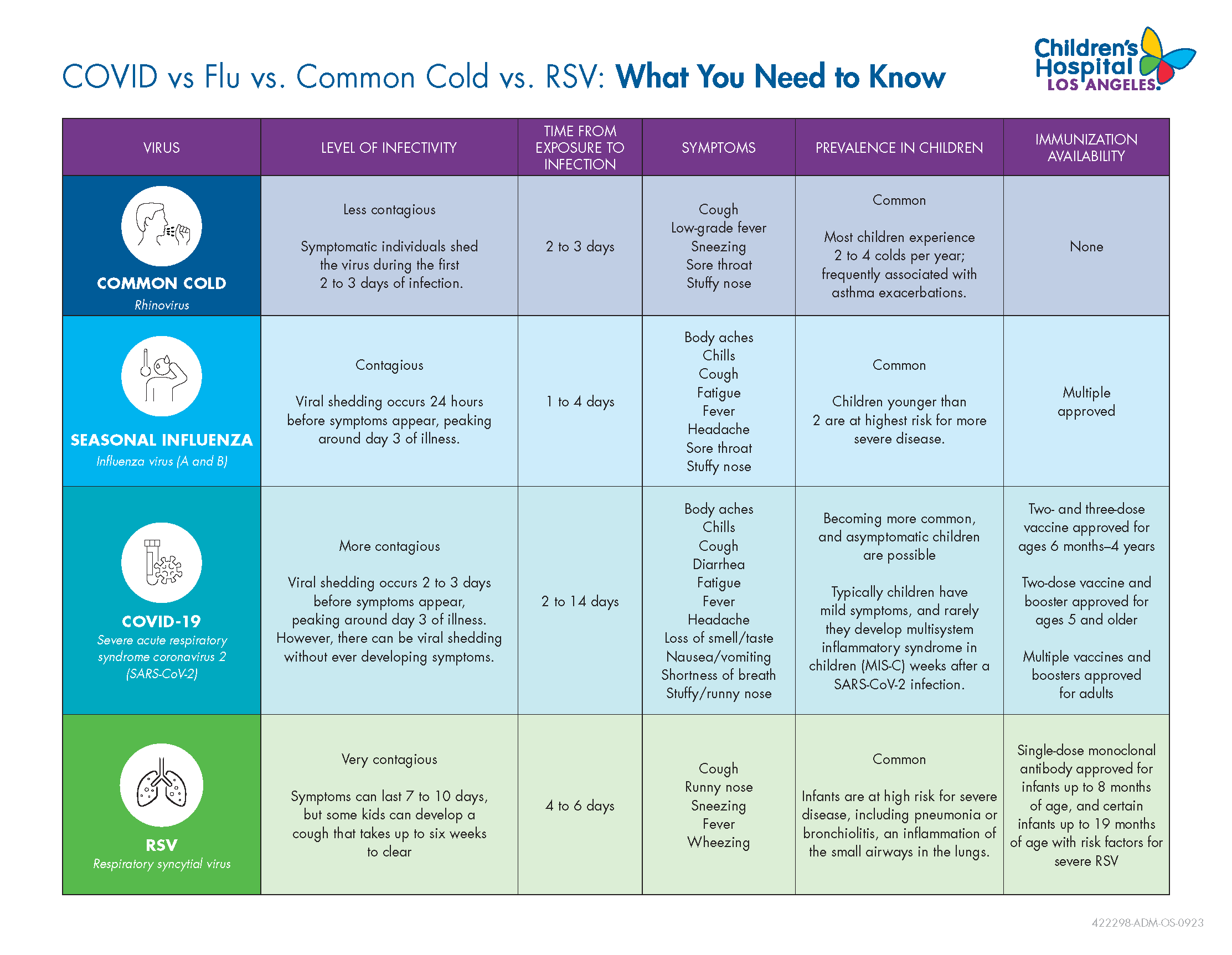
Because respiratory virus symptoms can present similarly, it is important to monitor and seek medical care for testing and treatment recommendations. The chart below from Children’s Hospital of Los Angeles, part of PPMD’s Certified Duchenne Care Center network, compares the different respiratory virus symptoms.
Medical Management
People living with Duchenne & Becker are especially vulnerable to the effects of the respiratory virusesflu, especially the pulmonary effects. If your child has symptoms of the flu, COVID-19 or RSV call your primary health care provider immediately!
It is important to note that antiviral treatment options will be different for influenza versus COVID-19, which is why it is important to get tested before starting treatments.
Influenza Testing & Treatment
Rapid diagnostic testing, which checks secretions in the throat for the influenza virus, is 50-70% accurate for diagnosing influenza. If the test is negative, most providers will send the specimen for culture just to be sure that there is no virus present. If the test is positive, starting an antiviral medication is recommended.
Antiviral medication should be started as soon as possible in the course of the illness and continued for five days.This medication works best if started within the first 48 hours after symptoms begin. However, it can still help even if started later, especially for people whose illness lasts longer or becomes more complicated. They can also prevent serious complications of the flu, like pneumonia.
There are three antiviral drugs for influenza recommended by the CDC:
- Oseltamivir (TamifluR): approved for children >2 weeks; available in pills or liquid
- Zanamivir (RelenzaR): approved for children >7 years; not recommended if there is underlying respiratory dysfunction; given via inhaler
- Baloavir (XofluzaR): single dose pill approved for early outpatient children >12 years
The most common side effects of any antiviral drugs are nausea and vomiting; Zanamivir (because it is inhaled) may cause bronchospasms (difficulty breathing with wheezing). Rare occurrences of neuropsychiatric events have been associated with Tamiflu.
COVID-19 Testing & Treatment
Viral tests look for a current infection with SARS-CoV-2, the virus that causes COVID-19, by testing specimens from your nose or mouth. This can be done with an at-home test or at your doctor’s office. It’s important to follow instructions carefully if doing the test at home, otherwise you may get a false result.
If you test positive for COVID-19 and have symptoms, even if they are mild, talk to your doctor about potential antiviral treatment options. It is important to never take medications or supplements that have not been prescribed or approved first by your doctor. Below are several FDA approved antiviral medications used to treat mild to moderate COVID-19 in people who are more likely to get very sick:
- Paxlovid (Nirmatrelvir with Ritonavir): approved for children and adults ages 12 years and older; must be taken within 5 days of when symptoms start; take by mouth
- Veklury (remdesivir): Approved for adults and children; must begin within 7 days of symptoms start; given as intravenous (IV) infusions at a healthcare facility for 3 consecutive days
- Lagevrio (Molnupiravir): approved for adults; must be taken within 5 days of when symptoms start; take by mouth
You can read more about treatment options for COVID-19 here.
This publication, representing many Certified Duchenne Care Centers, outlines consensus recommendations if a person with Duchenne or Becker were to be diagnosed with or suspected of infection with COVID-19, and guides physicians and caregivers on best practices for management and treatment.
Over the Counter Medications
You should always check with your primary health care provider and/or your neuromuscular provider regarding the safety and dosing of any medications. Over the counter medications that are generally safe for colds and flu can be found below. If you or your child has a fever over 104o F that is not responding to Tylenol (i.e. going down to at least 102o F within 1-2 hours of giving Tylenol), please ask your primary care provider and neuromuscular team if it is safe to use ibuprofen (AdvilR) and/or naproxen (AleveR). Be sure that the person that you ask is aware of ALL medications you are taking (including ACE inhibitors).
For children over 4 years, the following over the counter medications are generally safe for people with Duchenne & Becker to take:
- Tylenol (acetaminophen)
- Cough medicine without Sudafed – cough medicine with cough suppressant should be used if the cough is interfering with sleep; using cough medicine with cough expectorants, using Mucinex, maximizing hydration, and using the cough assist during the day may help minimize coughing at night
- Cough drops
- Mucinex (check with your pulmonologist; some pulmonologists caution against using Mucinex in patients with breathing dysfunction; the thinned secretions may cause aspiration of the secretions, which can lead to an increased risk for pneumonia)
- Saline nose drops/spray
For a list of safe and unsafe over the counter medications click here.
Create a Sick Day Plan
Because respiratory illnesses can come on quickly, it is important to work with you/your child’s neuromuscular team, including the pulmonologist, to create a sick day plan. This individual plan outlines what to do when ill, how to manage symptoms at home(including use of a cough assist machine), potential steroid stress dosing, and when to call and/or seek care. If you do not have a sick day plan, ask your neuromuscular team to create one at your next visit.
WHEN TO SEEK EMERGENCY CARE
Typical symptoms of respiratory viruses include fever, cough, sore throat, runny/stuffy nose, body aches, headache, chills, and fatigue. Occasionally symptoms may include vomiting and diarrhea. There may also be respiratory symptoms without fever.
There are warning signs that you/your child need emergency care immediately. These include:
In children
- Fast breathing or trouble breathing
- Bluish lips or face
- Ribs pulling in with each breath
- Chest pain
- Severe muscle pain (child refuses to walk)
- Dehydration (no urine for 8 hours, dry mouth, no tears when crying)
- Not alert or interacting when awake
- Seizures
- Fever above 104°F
- In children less than 12 weeks, any fever
- Fever or cough that improve but then return or worsen
- Worsening of chronic medical conditions
- Dark urine, indicating rhabdomyolysis
In adults
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest or abdomen
- Persistent dizziness, confusion, inability to arouse
- Seizures
- Not urinating
- Severe muscle pain
- Severe weakness or unsteadiness
- Fever or cough that improve but then return or worsen
- Worsening of chronic medical conditions
- Dark urine, indicating rhabodymyolysis
These lists are not all inclusive. Please consult your medical provider for any other symptom that is severe or concerning.
Steroid Stress Dosing During Illness
If you or your child is taking corticosteroids regularly, you may need a steroid stress dose during times of illness. This includes illness that causes fever, severe cold with fatigue, mild diarrhea, and/or mild vomiting. Additionally, If you or your child has missed 24 hours of corticosteroids, it is very important that you contact your neuromuscular provider for potential IM or IV steroid stress dosing.
Missing 24 hours or more of corticosteroids can result in acute adrenal insufficiency, which can be a life threatening condition. Your provider should refer to the PJ Nicholoff Steroid Protocol (download) for guidance on steroid stress dosing.
Coughing or Difficulties Breathing
Caring for your child’s lungs when they have a respiratory illness is critical. Information on caring for the lungs, the importance of cough, and assisting cough during an illness can be found on the PPMD website.
Pearls of Care
- Be sure all family members have been immunized against influenza and COVID-19.
- If you think you or your child with Duchenne or Becker has a respiratory illness , contact your primary care and/or neuromuscular provider immediately.
- Create a sick day plan with your neuromuscular team so you know what to do when ill, when to call, and when to seek emergency care
- Treatment recommendations should always come from your primary and/or neuromuscular provider
- Take recommended over the counter medications.
- Maintain cough and breathing.
- If you/your child are on corticosteroids, it’s important to understand when steroid stress dosing may be needed. You should refer to the PJ Nicholoff Steroid Protocol and call your neuromuscular provider right away if you are unsure if a stress dose is needed.
- Go to the emergency room if necessary and remember to take all of your medications and equipment with you.
- Continue to do what you can to stay as healthy as possible.
ADDITIONAL RESOURCES
Watch Connect with the Experts: Protect your Lungs This Winter (2022)
Watch A Patient’s Take on Pulmonary Management (2021)